Devastating data from two new reports by the South Carolina Department of Health and Human Control (DHEC) "show a dramatic increase" in deaths of mothers and infants. The 2023 Infant Mortality Report shows the total number of infant deaths was "the highest in nearly a decade," with 416 deaths. In 2012 there were 435 infant deaths. According to the report, Black infants are "dying at a rate nearly 2.5 times that of White infants."
The second report, using data from 2018-2019, investigated "66 pregnancy-associated deaths from 2019"—the state's most recent data. The 2019 report from the South Carolina Maternal Morbidity and Mortality Review Committee (SCMMMRC) showed a 9.3% increase in maternal deaths directly related to "pregnancy itself from the year before." The pregnancy-related mortality rate in South Carolina is higher than the national average, "especially in non-Hispanic Black women."
 IMR in SC since 2012/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
IMR in SC since 2012/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
Why No Mention of mRNA Vaccination Status?
Given the growing evidence of harm to mothers and infants from the COVID-19 vaccines, a few questions come to mind. It is perplexing that the 2023 report on infant mortality never mentions maternal vaccination status as part of their data, even though the mRNA jabs have been available since early 2021.
It is also interesting to note that the newly released 2019 report on maternal mortality mentions in a "COVID-19 graphic sidebar" deaths related to COVID-19 status while highlighting that 100 percent of the mothers were unvaccinated. Obviously, that is true because jabs were not available in 2019.
Nevertheless, the same sidebar states that "all COVID-19 deaths through 2021 were investigated." The mRNA shots became available in 2021. Additionally, the paragraph to the left of the sidebar explains that the 2018-2019 data was based on 66 deaths from 2019. Makes sense.
However, which part of the SCDHEC 2019 report is correct—the information in the sidebar stating "all COVID-19 deaths through 2021 were investigated" or the paragraph next to it which indicates a "review of 66 deaths from 2019" were studied? There may be a reasonable explanation, but it doesn't seem to make sense looking at the report.
 2019 Report Released in 2023/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
2019 Report Released in 2023/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
Most disturbing is the fact that further down in the sidebar, SCMMMRC continues to recommend COVID-19 vaccination for "all pregnant or post-partum women" even though both maternal and infant mortality rates are markedly on the rise and there is growing evidence of harm or death to mothers and infants from the mRNA vaccines.
One might also ask if the data on infant mortality from 2020-2021 is now available; where is the data from the same time period for maternal mortality? And why, other than recommending the COVID-19 vaccine for mothers, does neither report mention the vaccination status of pregnant or post-partum mothers?
What the Data Says for Infant Mortality
Infant mortality rate (IMR), as defined by the 2023 DHEC report, means a live-born baby died before its first birthday as calculated per 1,000 live births. South Carolina uses this United States-recognized standard to reflect "the overall state of a population's health." The state has prioritized the reduction of IMR as part of its "Healthy People 2030" objective.
However, data from this report is far from encouraging, at least in South Carolina. The report states that "while the US IMR has been declining over the past several years, SC's rate increased overall 12.3% between 2020 and the end of 2021. Non-Hispanic Black infants showed the sharpest rise in infant mortality. Infant mortality rates (IMR) as a whole increased markedly (6.8%) from 2020 through 2021. According to this DHEC report, IMR for infants born to Black mothers has increased by 39.6% since 2017.
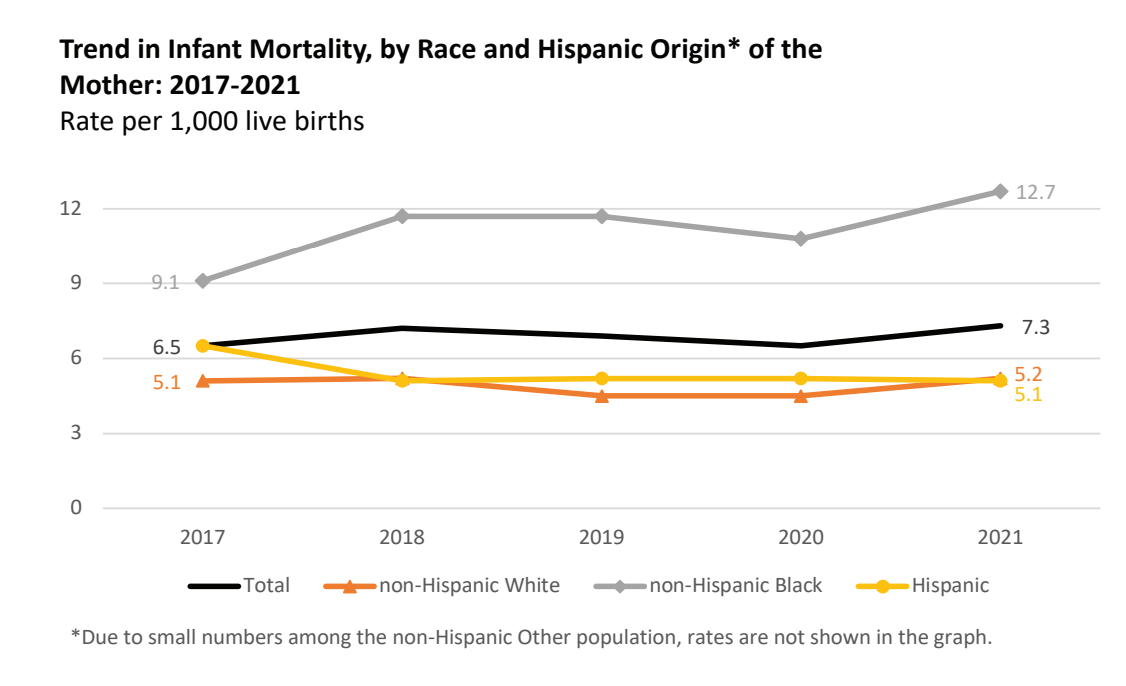 South Carolina Infant Mortality Rate/ 2017-2021/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
South Carolina Infant Mortality Rate/ 2017-2021/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
In addition, the "IMR increased across both the neonatal and postnatal periods in 2021. Most of the increase is attributed to a 23.8% increase in postneonatal mortality between 2020 and 2021. The Neonatal mortality rate increased by 6.8% during the same period.
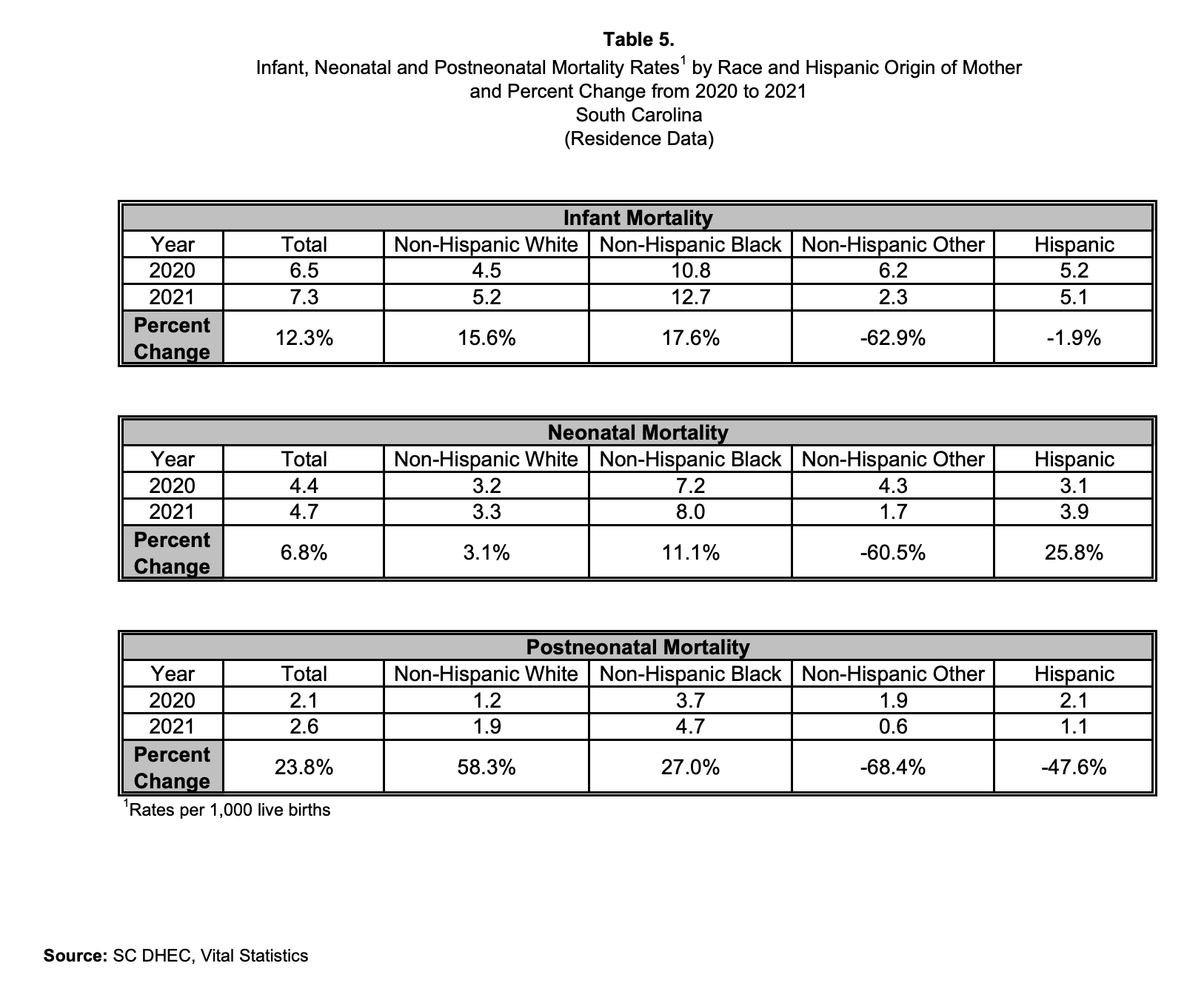 Table 5. Infant Mortality Rates/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
Table 5. Infant Mortality Rates/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
The three leading causes of infant death in South Carolina were:
 Leading Causes of IMR in SC/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
Leading Causes of IMR in SC/https://scdhec.gov/sites/default/files/Library/CR-012142-2021.pdf
SIDS ranked fourth, and accidents due to suffocation or strangulation in bed were the fifth-leading cause of infant deaths.
Notably, Dr. James Thorp, an OBGYN and fetal medicine specialist who sees upwards of 8,000 patients a year, has investigated the mRNA vaccines and their link to maternal, fetal, and infant health. He has used data from the CDC and Pfizer's internal data during his exhaustive investigation. Thorp has seen a "1200-fold increase in severe menstrual abnormalities, a 57-fold increase in miscarriage, a 38-fold increase in fetal death or stillbirth rates." He also found "15 other major pregnancy complications, all far exceeding the CDC and the FDA values of safety." Thorp believes pushing the vaccines has been the "greatest violation of medical ethics in history."
Thorp is seen speaking in one of the round tables hosted by Senator Ron Johnson (R-WI) concerning evidence about injuries and deaths from the lethal COVID-19 vaccines. Thorp says his patients are "the rate-limiting factor of future generations."
SCDHEC Data on Pregnancy-Related Maternal Deaths
A pregnancy-related (PR) death is defined in South Carolina's DHEC report as a death that occurs during or within one year of pregnancy from a "pregnancy complication, a chain of events initiated by the pregnancy, or a condition made worse by the pregnancy." A 2022 SCMMMRC review of 66 deaths from 2019 showed that 22 of the 66 deaths were pregnancy-related. Additionally, in 2019, investigators found a 9.3% increase in PR deaths. Notably, a cardiologist and a forensic pathologist were added to the committee members in charge of the report. This may be because of the uptick in cardiac complications associated with the vaccines, per a 2022 systematic review. The review states, "Myocarditis was the most commonly reported adverse cardiac event associated with mRNA COVID-19 vaccines."
Alarmingly, non-Hispanic Black women were again most likely to experience much higher mortality rates "than their counterparts"—67% higher. In 2018 and 2019, over 70% of PR deaths "occurred during the post-partum period," or within 42 days of delivering the baby.
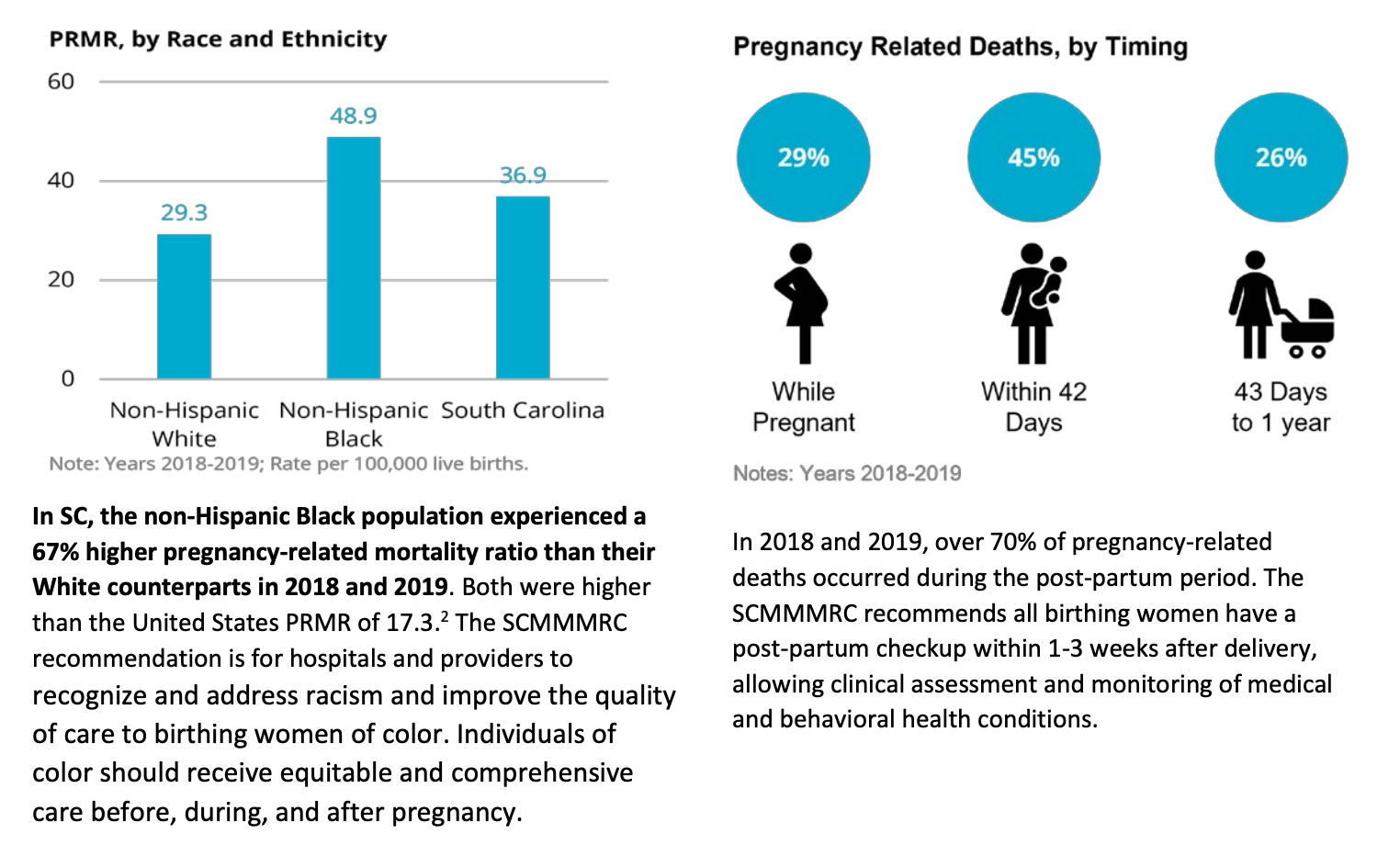 PR Deaths/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
PR Deaths/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
The leading causes of pregnancy-related deaths are cardiomyopathy, mental health conditions, hemorrhaging, cardiovascular conditions, and infections. In non-Hispanic Black women, the leading cause of PR death was cardiomyopathy. In non-Hispanic Whites, pregnancy-related deaths were most often linked to mental health issues. The report states that a vast majority of the deaths were preventable—81.8 percent in 2019. That statistic jives with the national statistic of 80%.
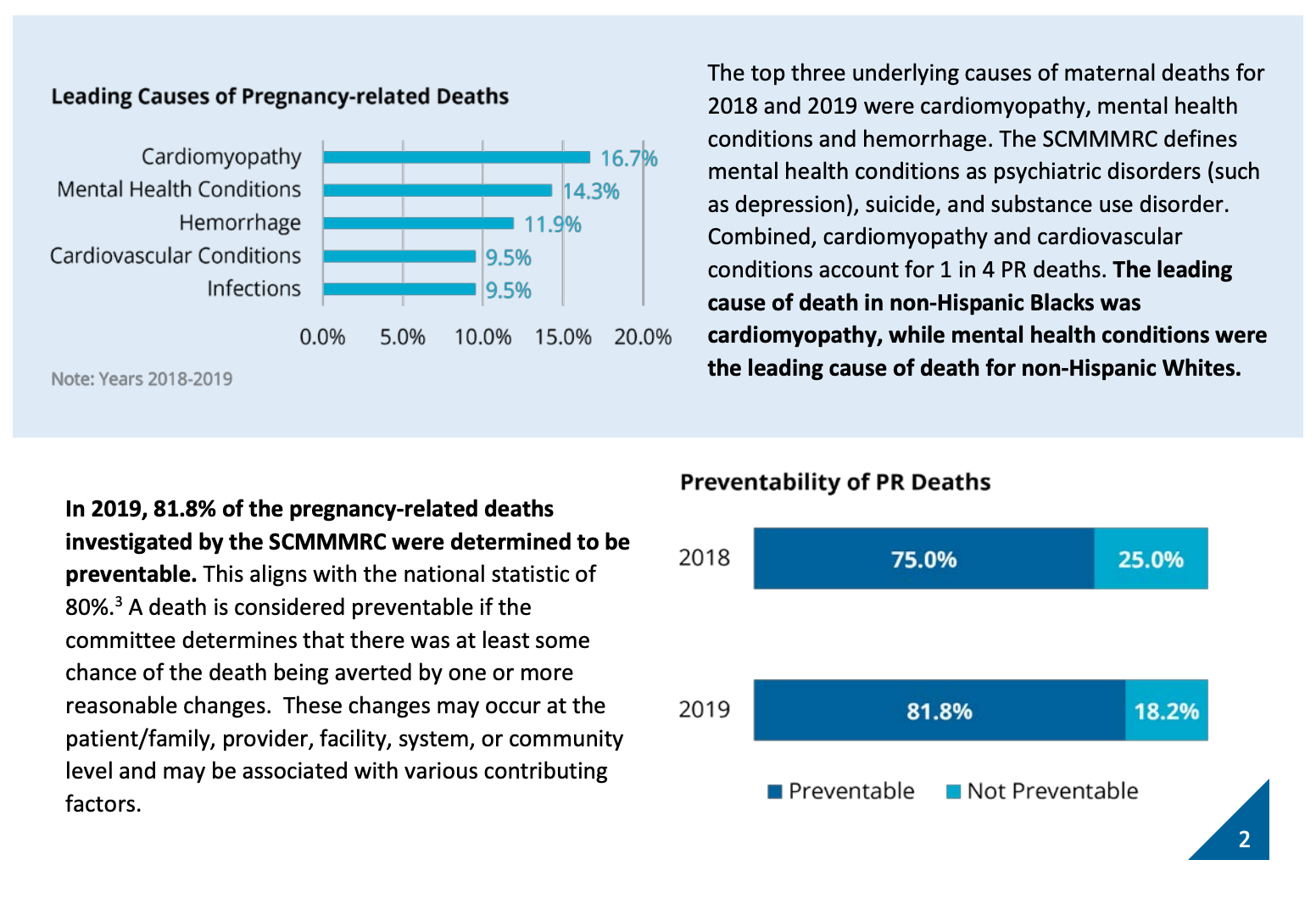 SC PR related Deaths/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
SC PR related Deaths/https://scdhec.gov/sites/default/files/Library/CR-013357.pdf
Contributing factors were also studied when looking at PR deaths. Discrimination ranked highest as a factor at 55.6%, followed by substance abuse, mental health, and obesity. The study also looked at maternal age, which has long been known to be a factor in PR-related deaths. In 2018-2019 in South Carolina, women aged 40-44 were 3 to 4 times more likely to experience a PR death than their younger counterparts, according to the report. Women who lived in rural areas of South Carolina were much more likely to die from PR-related deaths than those who lived in cities.
South Carolina expanded its post-partum Medicaid coverage to 12 months in 2018-2019. Medicaid was the leading payor source for prenatal care and delivery of women who suffered pregnancy-related deaths at 62.2% of those studied. The report recommended health care access as its number one priority for healthy pregnant women. Clinical intervention concerning hemorrhaging was second, followed by continuity of care.


