The Centers for Disease Control (CDC) revoked the emergency use authorization (EUA) for the Polymerase Chain Reaction (PCR) test on July 21. The test will be discontinued on December 31, 2021. The organization is now recommending that labs "implement one of the many FDA-authorized alternatives."
Notably, the CDC is now emphasizing the use of the Flu SC2 Multiplex Assay to help differentiate between Sars-CoV-2, Influenza A, and Influenza B. UncoverDC reported the importance of parsing the difference between Covid-19 and Influenza-Like Illness (ILI) back on April 5, 2020. Editor-In-Chief Tracy Beanz released a video explanation to accompany her above article on the subject and it can be viewed here.
"In preparation for this change, CDC recommends clinical laboratories and testing sites that have been using the CDC 2019-nCoV RT-PCR assay select and begin their transition to another FDA-authorized COVID-19 test. CDC encourages laboratories to consider adoption of a multiplexed method that can facilitate detection and differentiation of SARS-CoV-2 and influenza viruses. Such assays can facilitate continued testing for both influenza and SARS-CoV-2 and can save both time and resources as we head into influenza season. Laboratories and testing sites should validate and verify their selected assay within their facility before beginning clinical testing."
 SC2 Multiplex Testing/CDC
SC2 Multiplex Testing/CDC
According to itnonline.com, “If and when FDA EUA comes to an end, manufacturers of COVID-19 tests will need to seek regular FDA approval, which can require even more clinical evidence than what was required for an EUA.”
The FDA is, in fact, also revoking EUAs for SARS-CoV-2 tests developed by Gravity Diagnostics, Curative, and BioFire Diagnostics. Per Genomeweb.com, the Gravity Diagnostics tests received FDA EUA in June 2020. Gravity requested that the test be revoked because it was replaced with a better test in July 2020, a test that "provides better coverage of the SARS-CoV-2 viral RNA and internal workflow efficiencies."
The Curative-Korva SARS-Cov-2 Assay was authorized in April 2020. However, it was found to have a higher risk of false negatives than other PCR tests. KorvaLabs disagreed "the test had performance issues" but has now moved away from using the test at its lab.
The BioFire Respiratory Panel 2.1 received EUA from the FDA in May 2020. However, in March of 2021, it was "granted de novo clearance from the US Food and Drug Administration for its Respiratory Panel 2.1." According to GenomeWeb,
"The test is the first SARS-CoV-2 diagnostic to transition from an Emergency Use Authorization status and be permitted to be marketed beyond the public health emergency."
"In addition, this action also creates a new regulatory classification, "which means that subsequent devices of the same type with the same intended use may go through the FDA's 510(k) pathway, whereby devices can obtain clearance by demonstrating substantial equivalence to a predicate device," FDA said.
UncoverDC previously reported the PCR tests do not have the ability to detect viral load. If it cannot test for a viral load, it cannot tell you whether you have a viral infection. Additionally, the CDC has shifted the Cycle Threshold (CT) Value for the PCR test several times, most recently for the vaccinated, as reported by UncoverDC in May.
Furthermore, the FDA amendment from April of 2021 allows labs to use pooled testing. Excerpts from the FDA amendment regarding pooled testing can be found below:
 FDA Pooling and Serial Testing Amendment/FDA.gov
FDA Pooling and Serial Testing Amendment/FDA.gov
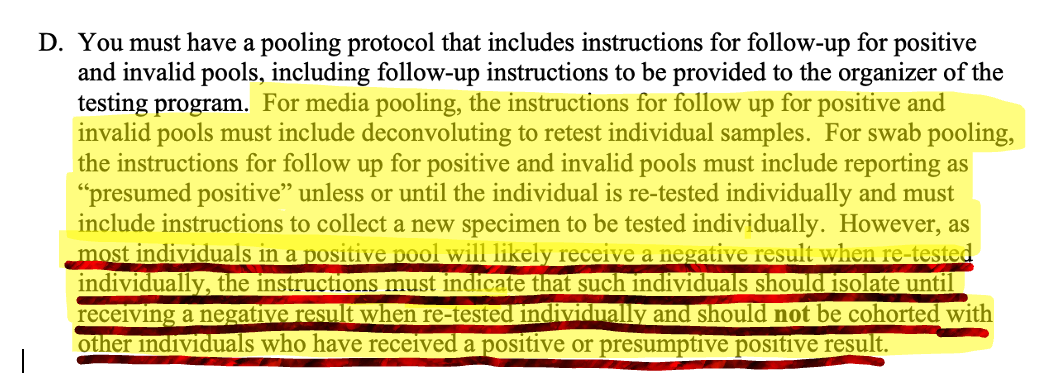 FDA Pooling Amendment/April 2021/FDA.gov
FDA Pooling Amendment/April 2021/FDA.gov
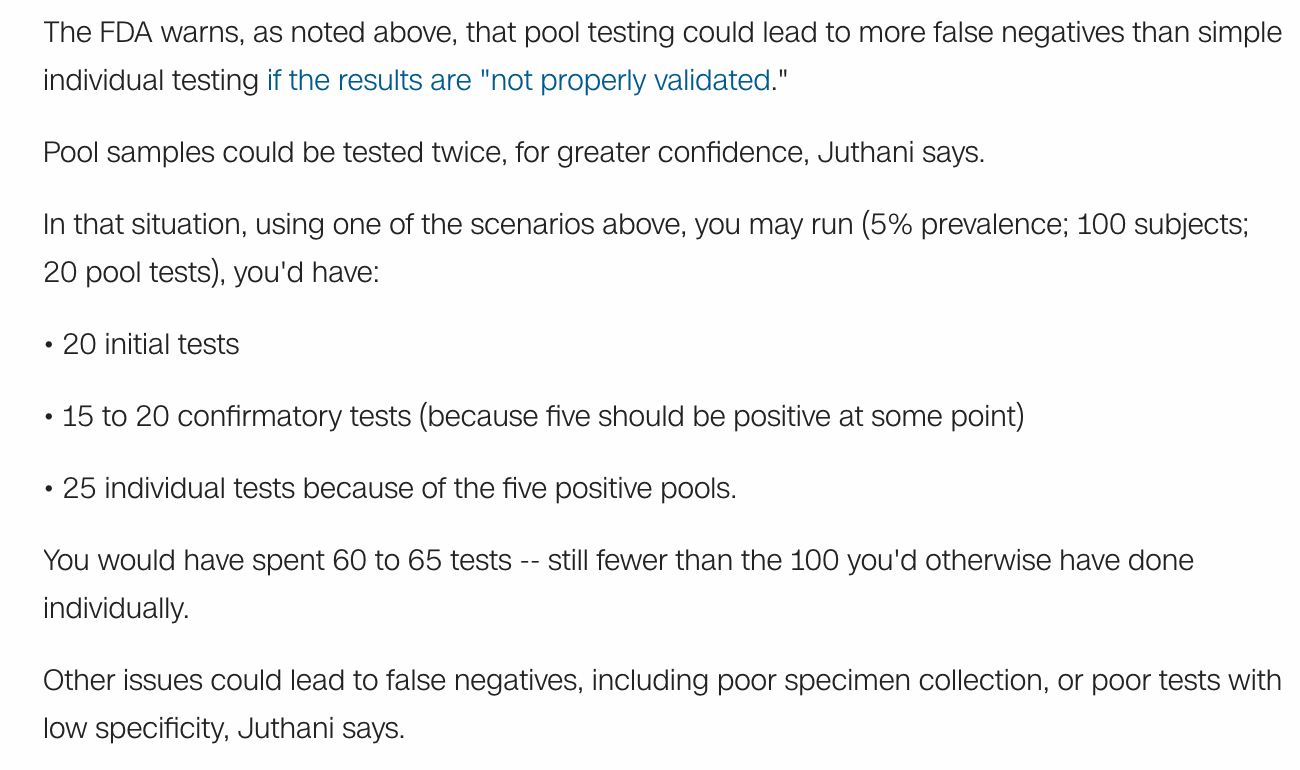
There are various reasons pooled testing is suggested. It saves time and money. A New York Times article in August 2020 discusses the pitfalls of using this approach to testing:
"Pooled testing only works when the vast majority of batches test negative. If the proportion of positives is too high, more pools come up positive—requiring each individual sample to then be retested, wasting precious chemicals..."
And later in the article:
"Experts disagree, for instance, on the cutoff at which pooling stops being useful. The Centers for Disease Control and Prevention’s coronavirus test, which is used by most public health laboratories in the United States, stipulates that pooling shouldn’t be used when positivity rates exceed 10 percent. But at Mayo Clinic, “we’d have to start to question it once prevalence goes above 2 percent, definitely above 5 percent,” Dr. Pritt said."
"And prevalence isn’t the only factor at play. The more individual samples grouped, the more efficient the process gets. But at some point, pooling’s perks hit an inflection point: A positive specimen can only get diluted so much before the coronavirus becomes undetectable. That means pooling will miss some people who harbor very low amounts of the virus."
A CNN report from July 2020 also discusses pooling at length. Throughout the article, there are statements that indicate that pooled testing, if done incorrectly, can have a negative impact.
 Pooled Testing/CNN/July 6, 2020
Pooled Testing/CNN/July 6, 2020
 Split Pooled Testing/Litvak
Split Pooled Testing/Litvak
Pool size, tainted samples, dilution of samples, disregard for prevalence in the community, test sensitivity and specificity, and failure to follow protocols for pooled testing are all significant issues with pooled testing per NIH research found here.
Most of the respected research indicates smaller pool sizes are better—pool sizes of 4 or less. Probes that test positive in the first stage must be retested in the second stage to reduce the occurrence of false positives. Nevertheless, pooled sample testing is common practice when tracking infectious diseases because it "reduces the cost of screening a large number of individuals."
The implications of PCR testing are profound in their effect. For example, a false-positive test has the power to produce fear, to isolate, to trigger lockdowns, quarantines, and more. There is evidence that there have been issues with quality control with regard to PCR testing. As Celia Farber reported for UncoverDC on April 7, 2020:
"In the US, we have all but abandoned classical diagnostic medicine in favor of biotech, or lab result medicine. This has been going on for a long time and is a dangerous turning. The “Corona test” is named with characteristic tech-tedium: “CDC 2019-nCoV Real-Time RT-PCR Diagnostic Panel.” That means it is a needle in a DNA haystack test. A PCR test."
“We need to quarantine everybody who’s positive. Next step. We need to do social isolation. It’s a mathematical model. And at the end you always win, right? So, in the end, the good guys win, and the pandemic is defeated. But there’s, there’s never been like an actual real pandemic since they built this machine. So, there’s this huge machine, it’s got a red button on it and it’s like if you ever detect a pandemic starting, you press the red button.."
While researching her article on PCR, Farber spoke with Canadian researcher, David Crowe.
"I conducted a two-hour interview with David Crowe– Canadian researcher, with a degree in biology and mathematics, host of The Infectious Myth podcast, and President of the think-tank Rethinking AIDS. He broke down the problems with the PCR based Corona test in great detail, revealing a world of unimaginable complexity, as well as trickery."
In another conversation about the PCR test, he told Farber "something unforgettable."
“So, we’ve essentially been taken over by the medical Taliban, if you like.”
I pressed him one last time:
“David, in conclusion, finish this sentence: “The PCR test for Corona is as good as…”
His reply made me laugh. I didn’t know I still could laugh.
“It’s as good as that Scientology test that detects your personality and then tells you; you need to give all your money to Scientology. “


